Rotator cuff tears may cause pain and weakness in the affected shoulder. Most people say they are unable to sleep on the affected side due to the pain. In some cases, a rotator cuff may tear only partially. Partial tears may be painful but you can still move your arm normally. Certain types of partial rotator cuff tears may not require surgical repair and your physician may want to consider non-surgical options that may include: limiting activities, anti-inflammatory medications, physical therapy or an injection of a steroid medication into the shoulder joint.
When the tendons of the rotator cuff are damaged, it can result in pain, weakness, and decreased shoulder range of motion. Night pain is common, and the pain will often radiate down the outside of the arm. Depending on severity of the tear, patient age, mechanism of injury, and health problems, treatment may include cortisone injections and physical therapy versus surgical repair. If a rotator cuff tear is too large to fix, a partial repair, superior capsule reconstruction, tendon transfer, or reverse total shoulder replacement can be performed to help improve function and decrease pain. Rotator cuff tears are described as acute/traumatic or chronic/degenerative. In each category, the tears may be further classified as partial or full thickness tears.
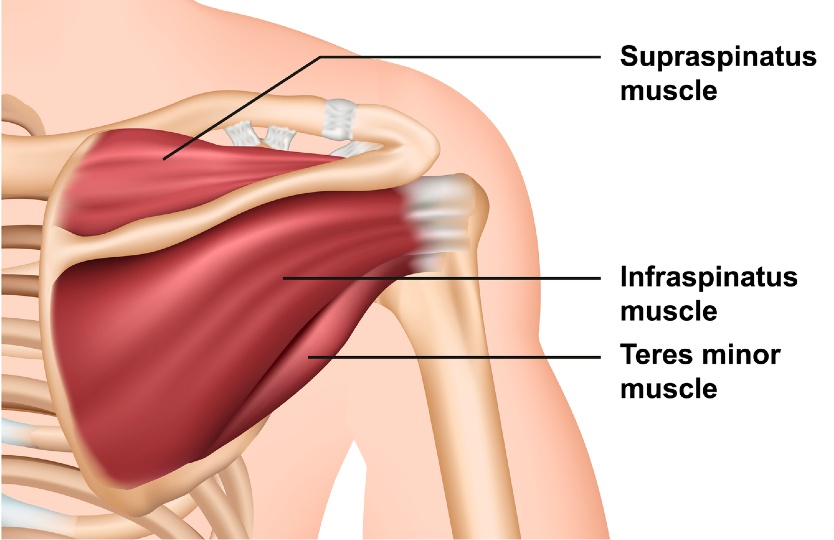
Our surgeons manage the entire spectrum of rotator cuff pathology from partial tears, full thickness tears, irreparable tears, and revision rotator cuff surgery. The rotator cuff is comprised of 4 muscles, the subscapularis, supraspinatus, infraspinatus, and teres minor. They originate off the shoulder blade and attach to the proximal humerus. They function to internally rotate, externally rotate, and elevate the arm. They also work to keep the humeral head centered in the socket of the shoulder blade. These tendons can become injured slowly over time from general use, or they can be acutely damaged from a trauma or lifting injury.
Impingement syndrome refers to the rotator cuff tendons rubbing or "impinging" on the undersurface of the acromion. This can lead to rotator cuff fraying, tendonitis or inflammation in the tendon, and subacromial bursitis. When the tendon is inflamed it results in pain, but typically not weakness. Non-operative treatments are usually successful; however, some people have significant hooking of the anterior acromion or develop spurs. If injections, therapy, and NSAIDs fail to alleviate pain, some patients benefit from surgical debridement and decompression; however, good results are less predictable than surgery for rotator cuff tears.
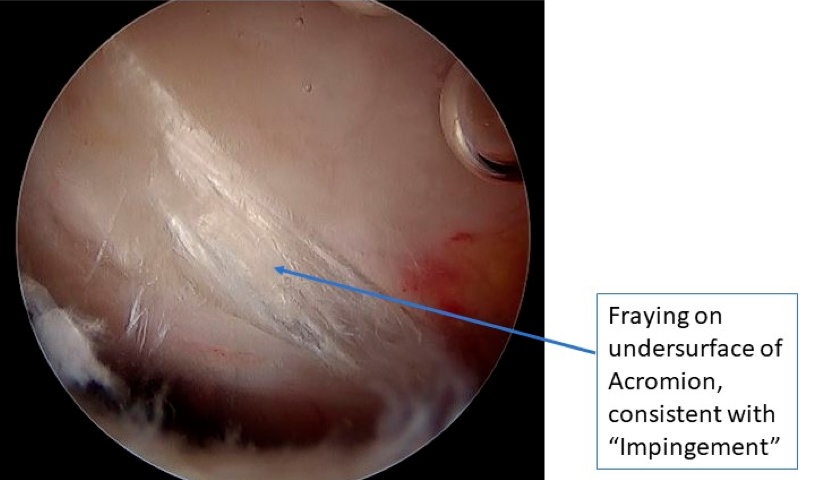
An arthroscopic image of an "impingement lesion" under the acromion.
Video animation demonstrating the concept of rotator cuff impingement.
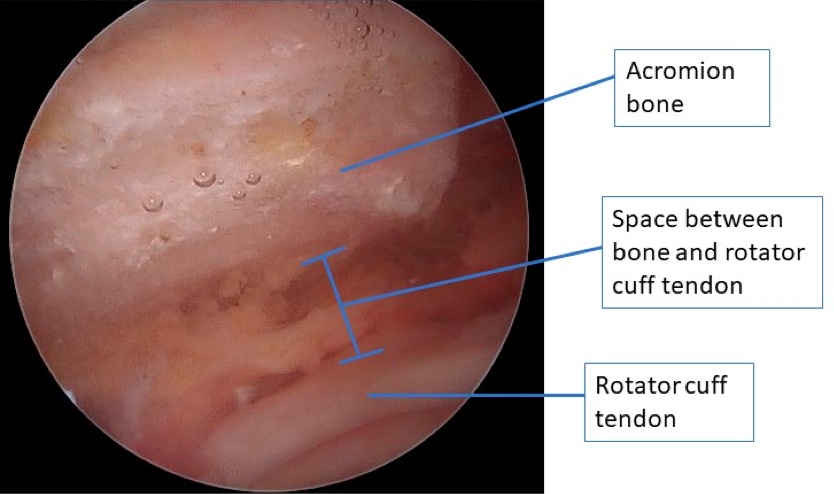
An arthroscopic image of the acromion before bone removal.
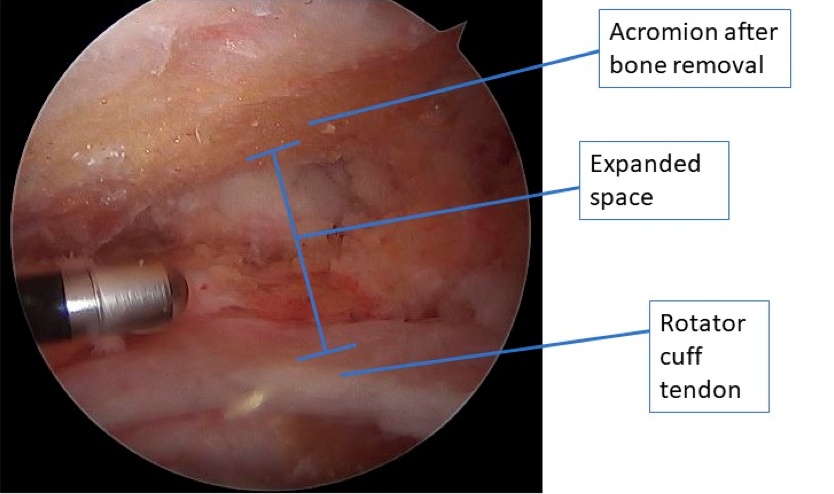
An arthroscopic of the acromion after bone removal.
A partial thickness rotator cuff tear involves only a portion of the rotator cuff fibers being torn, with some still being attached to the proximal humerus. These tears can be treated without surgery initially, which typically involves physical therapy, activity modifications, NSAIDs, and sometimes cortisone injections. When non-operative treatments fail to alleviate pain, then surgery can be performed.
If surgery is required, it may include debridement of the partially torn tendon or repair if the tear is deep enough. Partial rotator cuff tears can involve the bursal or articular fibers of the rotator cuff. If greater than 50% (roughly 6 mm) of tendon fibers are torn on the articular side at the time of surgery, the tendon is repaired. If less, only debridement is needed. If a tear involves the bursal surface, involvement of less than 25% of fibers (roughly 3 mm) requires only debridement, whereas tears deeper than 25% of the tendon width are often repaired.
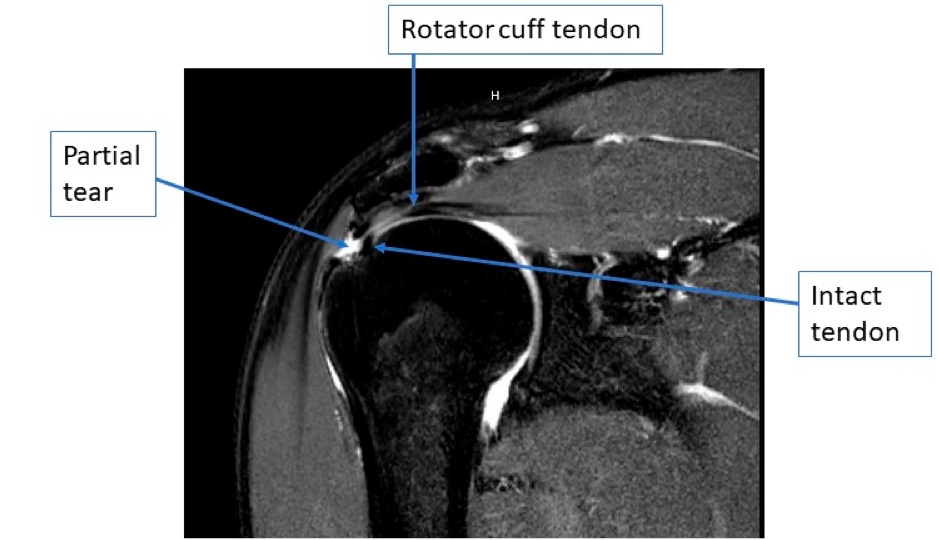
A coronal MRI image of a partial, bursal sided rotator cuff tear.
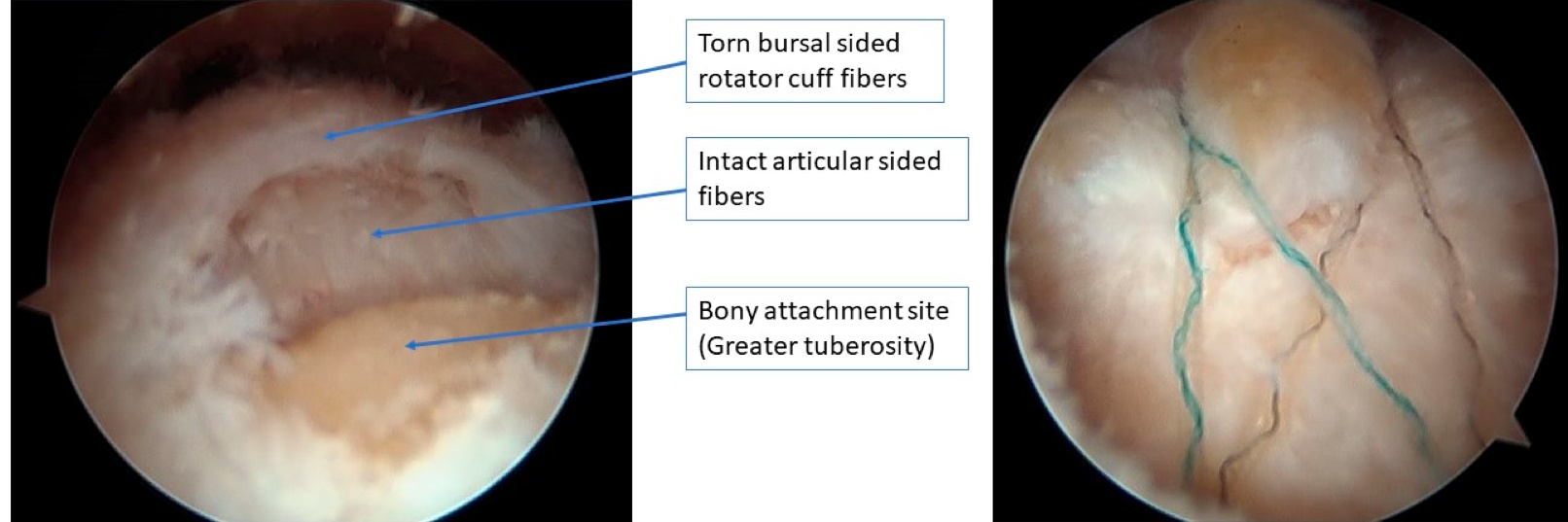
Arthroscopic images before and after bursal sided, partial rotator cuff repair. The image on the right demonstrated tendon mobilization and compression back down over the tuberosity bone.
A full thickness tear involves complete detachment of the tendon from the bone at the proximal humerus. It may develop slowly over time (chronic degenerative tears) or it may occur acutely from trauma. If it develops slowly over time (chronic-degenerative), patients are often able to compensate with the other muscles until the tear becomes too large and symptoms develop. Traumatic tears present with immediate weakness and pain.
Depending on patient age, type of tear, and medical problems, full thickness tears can be treated with cortisone injections, physical therapy exercises, or surgical repair. Treatments are largely individualized based on the patient, but in general, acute-traumatic full thickness rotator cuff tears are treated with surgical repair. Chronic-degenerative rotator cuff tears can be initially treated with non-operative options; however, full-thickness rotator cuff tears tend to enlarge over time, retract, and develop muscle atrophy, all of which decrease the chances of subsequent healing with surgery. Once the rotator cuff is torn, it does not heal on its own.
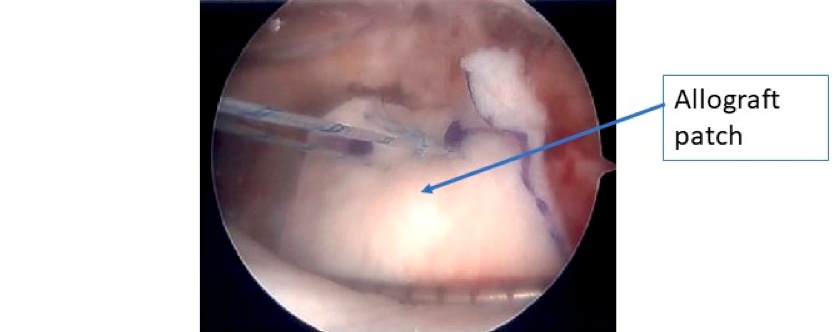
Our surgeons are also experienced with revision rotator cuff repairs and utilize advance arthroscopic techniques, including patch augmentation, in an attempt to facilitate healing.
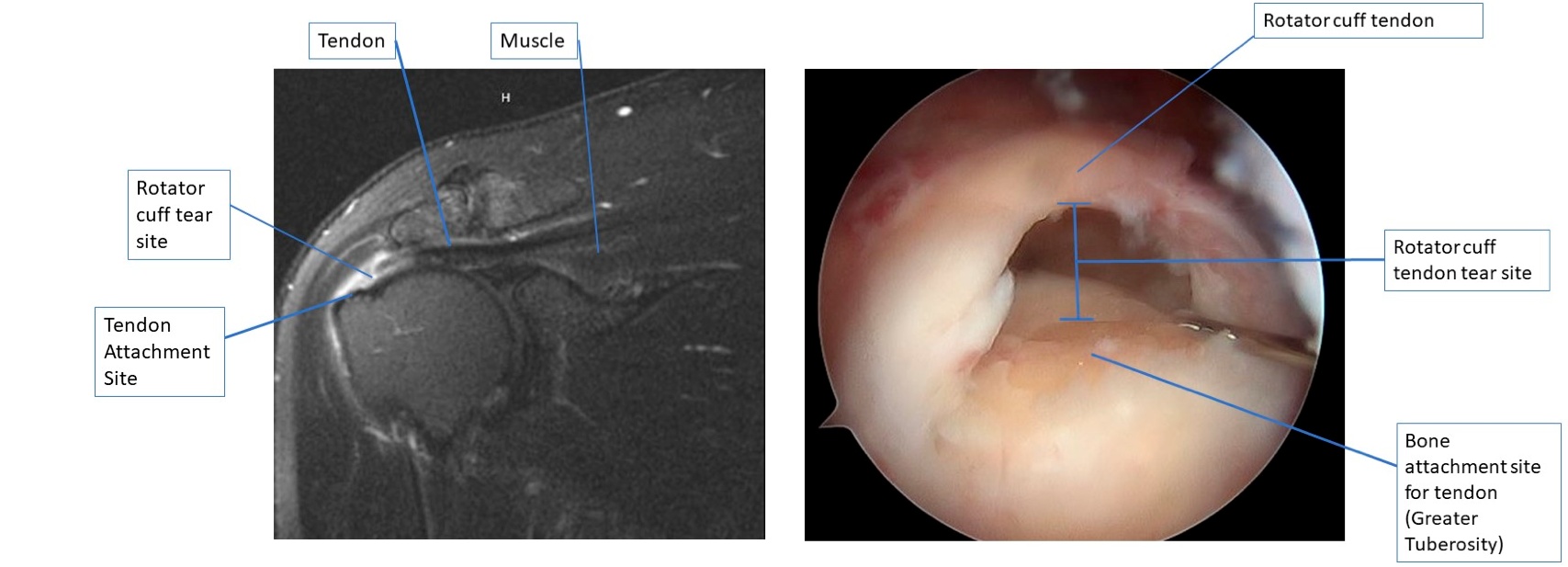
A coronal MRI image on the left of a full thickness rotator cuff tear, and the same tear when viewed with an arthroscopic camera on the right.

The coronal MRI far left, initial arthroscopic image middle, and final arthroscopic repair on far right of a full thickness rotator cuff tear.

Arthroscopic images of a revision rotator cuff repair using patch augmentation to help with healing.
A) Initial camera image of tear after preparation.
B) Standard repair of the recurrent rotator cuff tear.
C) Four additional anchors placed around the repair to hold down the graft.
D) Final image after graft has been tied down securely over the traditional rotator cuff repair.
When rotator cuff tendon tears become too large to repair, and non-operative treatments fail, there are several surgical options. These options are often based on a combination of surgeon preference, patient age, patient expectation, and overall patient health. Options include partial tendon repair, superior capsule reconstrution, tendon transfers, and reverse shoulder arthroplasty. Our surgeons are routinely performing superior capsule reconstruction for younger patients, and reverse shoulder replacement for older patients.
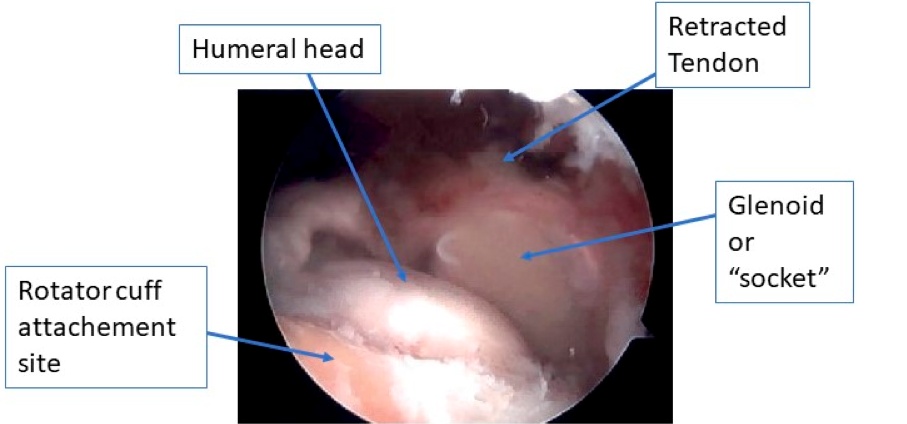
Arthroscopic image of a massive rotator cuff tear, not repairable by conventional techniques.
Arthroscopic image of the superior capsule reconstruction graft being introduced into the shoulder.
Final superior capsule reconstruction graft secured with suture anchors to the glenoid and greater tuberosity.
Video animation by Arthrex demonstrating a superior capsule reconstruction procedure.
In general, the larger the tear, the more weakness it causes. A complete tear generally makes it impossible to move the arm normally. It can be difficult to raise your arm away from your side by yourself. A complete rotator cuff tear will not heal and will require surgery if your goal is to return your shoulder to optimal function.
The surgery is done as an outpatient under general anesthesia and will take approximately 1 ½ hours. You may also receive a nerve block injection into your shoulder which will help with pain for several hours following the surgery. The surgeon will make approximately 3-5 small incisions (1/4 inch long) along the front, back and side of your shoulder. He will use these incisions to insert the arthroscope and several other tools. The arthroscope is a small camera device that allows the surgeon to look into the shoulder joint. He can insert tools to trim and remove the degenerative tissue and bone. The torn rotator cuff tendons are repaired by inserting suture anchors into the bone allowing for a strong attachment of the tendon to the bone. This will keep the tendon close to the bone allowing it to heal back to the bone.
You will awaken with a bulky dressing on your shoulder and a sling/immobilizer in place. Once you are awake, taking fluids, and are in stable condition, the IV will be removed and you will be discharged.
The nerve block you may have received during surgery will generally minimize pain for about 12-18 hours after surgery. The use of oral pain medications will be needed after the block has worn off. Expect significant pain for the first few days after surgery. The use of ice to your shoulder for the first week is very important. The bulky surgical dressing can be removed after 24-72 hours, depending on your physicians’ preference. You may then shower but do not submerge your shoulder in water. Remove your sling but keep your arm close to your side while showering. Do not apply lotion or antibiotic ointments to your incisions. You may keep your incisions open to the air if they are not draining, or apply clean dry band aids daily. You may be more comfortable resting or sleeping in a recliner type chair. You will have an appointment to see your surgeon in the office 2 weeks after surgery and any sutures will be removed. It is very important that you only remove your sling/immobilizer for showering and for passive exercises for the first 4 to 6 weeks.
It is important that your elbow stay close to your side when your sling/immobilizer is off for the first 6 weeks after surgery. Your surgeon will advise you when he wants you to begin formal physical therapy, which could begin immediately following surgery or not until 6 weeks after surgery. Rehabilitation after rotator cuff surgery can be a slow process. Getting the shoulder moving with simple passive exercises as soon as possible is important, however this must be balanced with the need to protect the healing tissues with the use of the sling/ immobilizer. The first 12 weeks following surgery are focused on regaining motion in your shoulder with a progression in exercises/therapy. You will not begin any strengthening or resistance type exercises until 12 weeks following surgery.
For additional information about this procedure, including what to do to prepare for your surgery and at-home instructions, we have included this complete patient eduction sheet as a pdf to view, download and print: